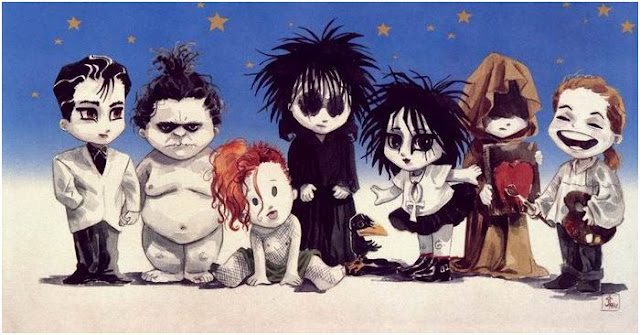
Rose knows when her mother, Poly comes over she talks about her seven grandchildren that have sleep problems. Children sleep disorders are very common. I’ve talked about Batboys issue of bed wetting or enuresis. Dawg not only doesn’t like to wear clothes, he suffers from sleepwalking or somnambulism. The cute girls, Cristie and Catie, have to sleep with their parents a behavioral sleep problem known as Co-sleeping. Morpheus has night terrors, while his sister Iris suffers from narcolepsy. Vail who wants to be called Nightshifter has child obstructive sleep apnea.
Most sleep problems are outgrown but obstructive sleep apnea (OSA) is a frequently missed diagnosed in children and often is cured by removing the tonsils and adenoids. Behavioral sleep problems such as Co-sleeping can be overcome with parental interventions.
Sleep problems in children concern parents as the children usually are unwilling to go to bed, fight falling asleep and wake up during the night. Sometimes defining a sleep disorder is difficult because sleep patterns vary in each developmental stage. It isn’t abnormal for a two month old to wake up during the night, but it is considered uncharacteristic in a two year old. Sleeping habits vary with families, as one family may consider a sleep behavior as normal while another may consider it a problem.
What is normal sleep in children? Infants under the age of six months spend 50% of their sleep in REM or rapid-eye-movement, compared to 20% in adults. Infants also enter REM faster than adults resulting in shorter sleep cycles. Parents are eager to get a child to sleep through the night because during the first six months they suffer from sleep deprivation themselves. A rule of thumb, frequency of night waking start at 100% for newborns and tapers off to 20% by the time they are six months. Infants sleep is about equal during the day and night.
Not until an infant is six months will they complete the four stages of sleep which is a mature sleep pattern. While the infant is developing a normal sleep pattern their nighttime sleep will increase and their daytime sleep decrease. This development will last for the first three years and by the age of four they will no longer need a daytime nap. One in three four year olds will still wake up during the night and will require a parent to help them go back to sleep or allow them to sleep in their bed. Usually when a four year old wakes through the night it is due to an immature central nervous system and is generally outgrown in time.
Those that suffer from pavor nocturnus (night terrors) like Morpheus find that it occurs approximately 90 minutes into stage 3 or 4 Non-REM sleep. Morpheus will suddenly sit up and scream. His parents have to console him for at least 30 minutes before they can get him to go back to sleep again. Night terrors usually occur in children three to eight years of age. Night terrors are different than nightmares as the child usually doesn’t remember what they were dreaming. Night terrors are more likely to occur when the child is stressed or overtired and usually when these issues are alleviated they will stop. In some cases children have been prescribed valium to relieve night terrors.
Dawg will get up, open his “unseeing” eyes and walk through the crypt. Somnambulism or sleepwalking occurs more often in boys than girls and may be associated with somnilquy or sleep talking. The speech is rarely intelligible as it is mumbled and slurred. Most sleep walkers are of school age therefore they have a potential to harm themselves. As with Dawgs case his parents have to make sure he doesn’t go outside in the sun. Make sure they are sleeping on the first floor and secure the home with additional locks. Never shake, slap or shout at a sleepwalker as parents should keep interventions at a minimum. This disorder is usually outgrown by adolescence and doesn’t required medical attention.
In one study parents kept a sleep journal of the time their child would show signs of sleepwalking and would gently wake the child and kept them awake for five minutes before letting them resume sleep. The study found that this technique stopped sleepwalking in more than 80% of the children.
Comparison of Night Terrors and Nightmares
Factor | Sleep Terrors | Nightmares |
Age | 3 to 8 years | Any age |
Gender | Male predominance | Either |
Occurrence in sleep cycle | NREM | REM |
Arousal? | No | Yes |
Memory for event | None | Yes |
Exacerbated by stress | Yes | Yes |
REM = rapid eye movement; NREM = non-rapid eye movement.
Batboy my bed-wetting nephew has the most prevalent and persistent sleep problem in children. Nocturnal enuresis, or bed-wetting, is classed as primary when the child has never been persistently dry through the night and as secondary when the child starts wetting the bed after one year of continence. Enuretic children have been found to have a lower functional bladder capacity (the volume of urine a bladder can hold before starting to empty) than children without enuresis, although their true bladder capacity is no different. Also bed-wetting more often than not will occur during Non-REM sleep. Some parents believe that these children have a harder time waking up during Non-REM sleep and know they have to go or are going. But studies have found they are not any more difficult to waken then child that don’t wet their bed.
More likely any in-depth diagnostic work-up will result in simply a sleep related enuresis that can be eventually stopped with age and behavioral interventions. Limit liquids in the evening, waking the child to use the bathroom before the parents go to bed or using a bed-wetting alarm may help. There are some medications such as Tofranil or DDAVP your doctor can prescribe. There are many books and devices you can research on the internet that may assist you with your child’s continence training.
Vail or umm..Nightshifter has obstructive sleep apnea (OSA) which is thought to affect 1 to 3 percent of children. Symptoms include snoring, difficulty breathing during sleep or mouth breathing during sleep. Parents of infants with significant OSA have reported difficulty with feeding. OSA in children is frequently caused by enlarged adenoids and tonsils. Other causes include craniofacial abnormalities, obesity and neuromuscular disease. Some allergies cause snoring and OSA. Usually OSA is associated with developmental delays as older children have learning and behavior difficulties including ADHD.
A child with OSA is usually seen by a sleep specialist and has a sleep test to determine the cause and severity. Most children have their tonsils and adenoids removed to relieve their symptoms. If OSA is caused by other than adenoids and tonsils may use a continuous positive airway pressure (CPAP) machine to alleviate their OSA.
Iris who suffers from narcolepsy is on the verge of adolescence. As narcolepsy is uncommon in children but may sometimes occur in adolescence. The predominant symptom is excessive sleepiness during waking hours and great difficulty waking up. When Iris is awoken she is often confused and verbally abusive. Some children benefit with regularly scheduled naps while others need stimulant medication. Narcolepsy is a lifetime sleep disorder and children should be under a sleep specialist care.
Co-sleeping is the term given to parents and children sharing the same bed as in Cristie and Catie’s situation. Many find that this is a bad sleeping habit which is very hard to break as it may interfere with the normal development of their independence.. Others support co-sleeping as it leads to children that feel secure and loved. Co-sleeping is common as 35 -55% of preschoolers and 10 -23% of school age children sleep with their parents. The U.S. Consumer Product Safety Commission recently published the results of a review of hazards associated with children placed in adult beds. The eight-year survey period contained 515 deaths in children younger than two years. Approximately one fourth of the deaths were due to an adult rolling over onto a child causing suffocation or strangulation.
Because of the prevalence of children sleep disorders, questions should be asked about your child’s sleep behavior and habits with every well-child doctor’s visit. Your pediatrician should use this time to let you know how a healthy sleep pattern is as important as any other health matter.
Good Day,
Rose Sheepskill

No comments:
Post a Comment